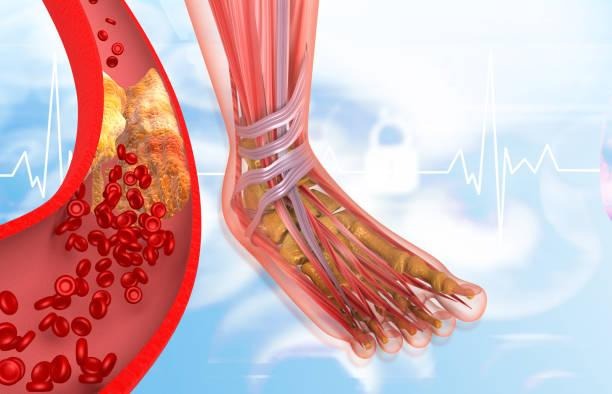
Medically, inflammation of superficial veins is known as superficial thrombophlebitis, where the veins close to the skin surface become inflamed due to blood clot formation. This usually happens in the legs but may also be present in the arms or neck.
Although it is not typically serious in most cases, early signs must be identified to prevent further complications and seek prompt treatment. Acquiring an understanding of the early signs provides a prompt opportunity to take action and reduces the risks associated with vein inflammation.
What is Superficial Vein Inflammation?
Superficial thrombophlebitis refers to the inflammation of superficial veins, characterised by swelling and irritation of the veins just beneath the skin surface. This is often due to the formation of a blood clot in the superficial veins, which causes swelling and redness in localised areas.
The affected vein becomes tender to the touch and may feel hard or like a cord. This differs from deep vein thrombosis, in which the involvement of deeper veins places patients at a higher risk for complications.
Common Early Signs to Recognise
It is imperative to recognise superficial vein inflammation early to enable effective management. Early symptoms of the condition include:
- Pain and tenderness are common in the affected veins, which may be painful or tender to the touch. Pain can be increased by pressure or movement.
- Erythema: The involved area usually presents with localised redness tracking along the distribution of the vein.
- Swelling may be visible around the inflamed vein, often accompanied by warmth in the area.
- Skin Warmth: The skin overlying the inflamed vein may feel distinctly warmer than the surrounding areas.
- Firm or Cord-like Vein: It may feel hard, thickened, or like a cord under the skin when the vein has become inflamed.
- Pruritus or a sensation of burning may also occur at the site in some instances.
- Skin discolouration: When inflammation of a vein occurs, the skin above the vein can darken or thicken.
These symptoms tend to develop gradually, but in some instances-particularly in those associated with vein injury or intravenous catheter usage-they can even occur suddenly.
Who is at Risk?
The following factors increase the risk of superficial vein inflammation:
- Long periods of inactivity, bed rest, or sitting, especially during long trips
- Conditions affecting the veins, such as varicose veins, are commonly known as varicose veins.
- Injury or trauma to a vein, including following surgery or medical intervention
- Use of intravenous lines or catheters
- Pregnancy and any form of hormonal changes, including birth control pills.
- Cancer or clotting disorders that increase the risk of blood clots
- Sedentary lifestyle and obesity
- Advanced age, especially those over 60 years
- Previous episodes of thrombophlebitis or deep vein thrombosis
- Knowing these risk factors may help both individuals and clinicians to show vigilance for early warning signs.
Importance of early detection and treatment
Early diagnosis of superficial vein inflammation can prevent the further development of symptoms and reduce the incidence of complications, including the extension of clot formation or infection.
Although superficial thrombophlebitis is usually self-limiting and may resolve without serious harm, it causes significant discomfort and requires treatment to alleviate symptoms.
Treatment usually involves one or more of the following:
- Pain medicines may include NSAIDs.
- Warm compresses to reduce pain and inflammation
- Compression stockings that allow for improved blood flow to the affected limbs
- Elevation of the affected limb to decrease swelling
- Avoid long periods in one position; encourage mild exercise
When the risk of clotting is high or symptoms are worsening, doctors may prescribe blood thinners, investigate underlying conditions, or both.
When to Seek Medical Attention
Though many cases improve with home care, medical evaluation is essential if you notice:
- Increasing pain or swelling
- Significant amount of redness or warmth spreading bigger than the initial area
- Hard, cord-like veins are becoming more prominent
- Fever or chills, which indicate infection
- Signs of deep vein thrombosis, including swelling of the entire limb, severe pain, or shortness of breath
The aim of early consultation is to rule out severe conditions and provide guidance on appropriate treatment.
Role of Medications Like Thrombophob
Such medications useful in superficial vein inflammation management are those that reduce inflammation and prevent the further development of a clot.
Thrombophob, one of the effective options, helps maintain vein health by minimising the development of clots, thereby relieving symptoms. Medication of this kind should be used under the supervision of a doctor for effectiveness and safety.
Preventive Measures
Preventive measures for superficial vein inflammation focus on reducing identifiable risk factors. Avoid a sedentary lifestyle; avoid sitting or standing continuously for long periods. Manage body weight and maintain cardiovascular health. Stay hydrated and avoid smoking.
The use of compression stockings is recommended if varicose veins or blood clotting issues are a concern. Follow medical recommendations in view of hormone therapy or birth control pills. These lifestyle habits can help contribute to healthy veins and reduce the risk of inflammation.
Summary
Superficial vein inflammation, or superficial thrombophlebitis, is a relatively common condition characterised by painful, red, swollen, and tender superficial veins. At the initial stage, it may exhibit symptoms of localised warmth, firmness of the veins, and itching sensations, which must not be neglected.
Recognition of risk factors and efficient prophylaxis may forestall complications and improve quality of life. If symptoms worsen, a timely consultation with a doctor is necessary. Drug administration, like Thrombophob, along with supporting therapy, can be helpful.
Disclaimer: This article is for general information and should not be used as a substitute for professional medical diagnosis or treatment. For diagnosis and treatment appropriate to your condition, always see a healthcare professional. Do not start or stop medication without seeking medical advice.